Merit-based Incentive Payment System (MIPS)
←VIEW BIGGER
45% Quality
25% Promoting Interoperability
15% Clinical practice improvement activities
15% Resource Use
MIPS eligible clinicians are required to participate and submit their data to avoid -9% of payment adjustment.
2020 Performance Flexibility
Due to the impact of the COVID-19 pandemic, clinicians can file for exceptions and use the Extreme and Uncontrollable Circumstances policy to allow clinicians, groups, and virtual groups to submit application requisitions of one or more MIPS performance categories.
QPP Exceptions
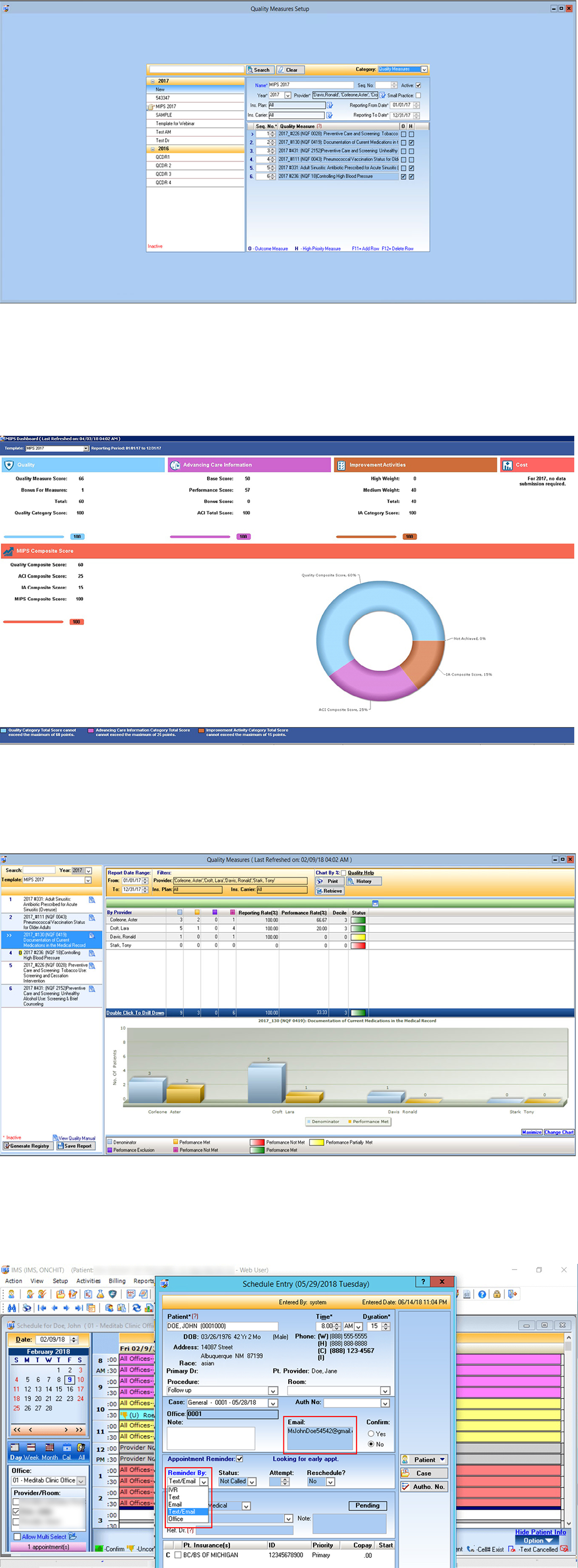
Quality Measures.
For the 2020 performance year, the Quality Performance Category will be worth 45% of your final score. Eligible Clinicians (ECs) must select 6 individual measures of which 1 must be an outcome measure or a high priority measure.
- If less than 6 measures apply, then ECs will report on each applicable measure. Eligible Clinicians may also select a specialty specific of measures
- Small practice bonus of 6 points for MIPS eligible clinicians in small practices who submit data on at least 1 quality measure. A small practice is defined as 15 or fewer eligible clinicians
- You can also receive up to 10 additional percentage points based on your improvement in the Quality performance category from the previous year.
2020 performance year requires a 70% data completeness threshold
- Measures that do not meet the data completeness criteria earn 1 point. Small practices continue to receive 3 points
- Updated the definition of high priority measures to include opioid related measures.
Review the available Quality measures here.
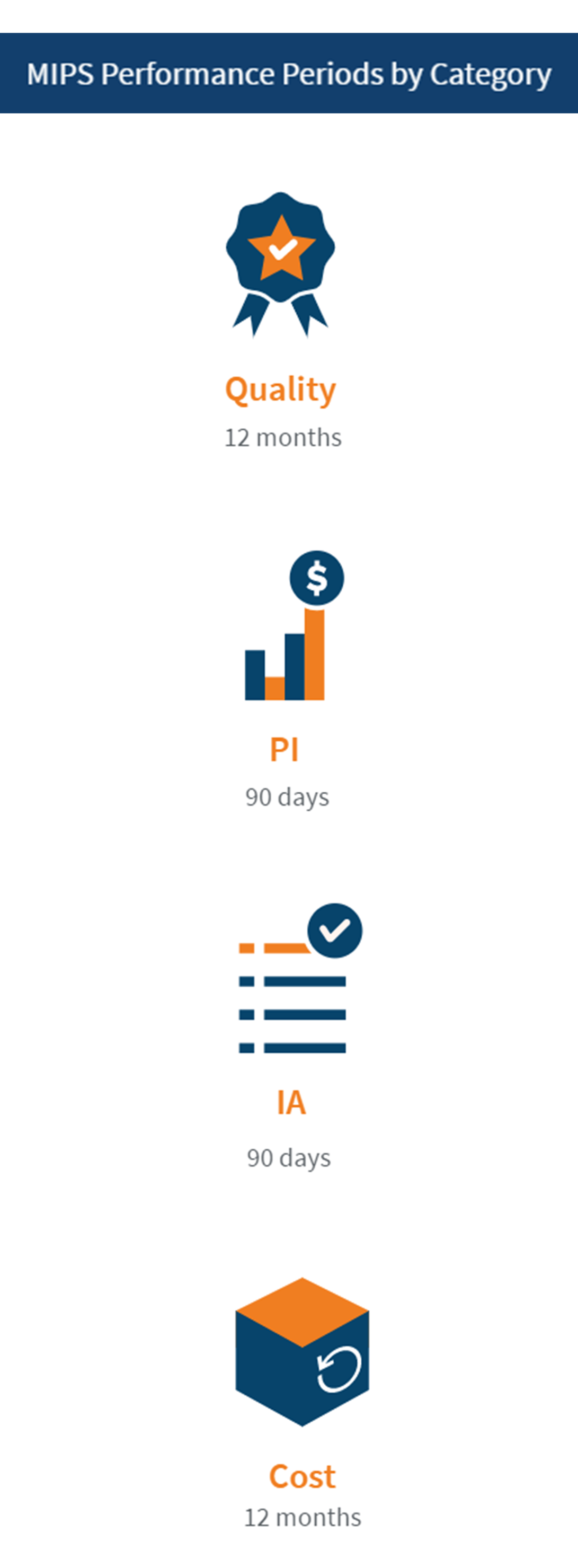
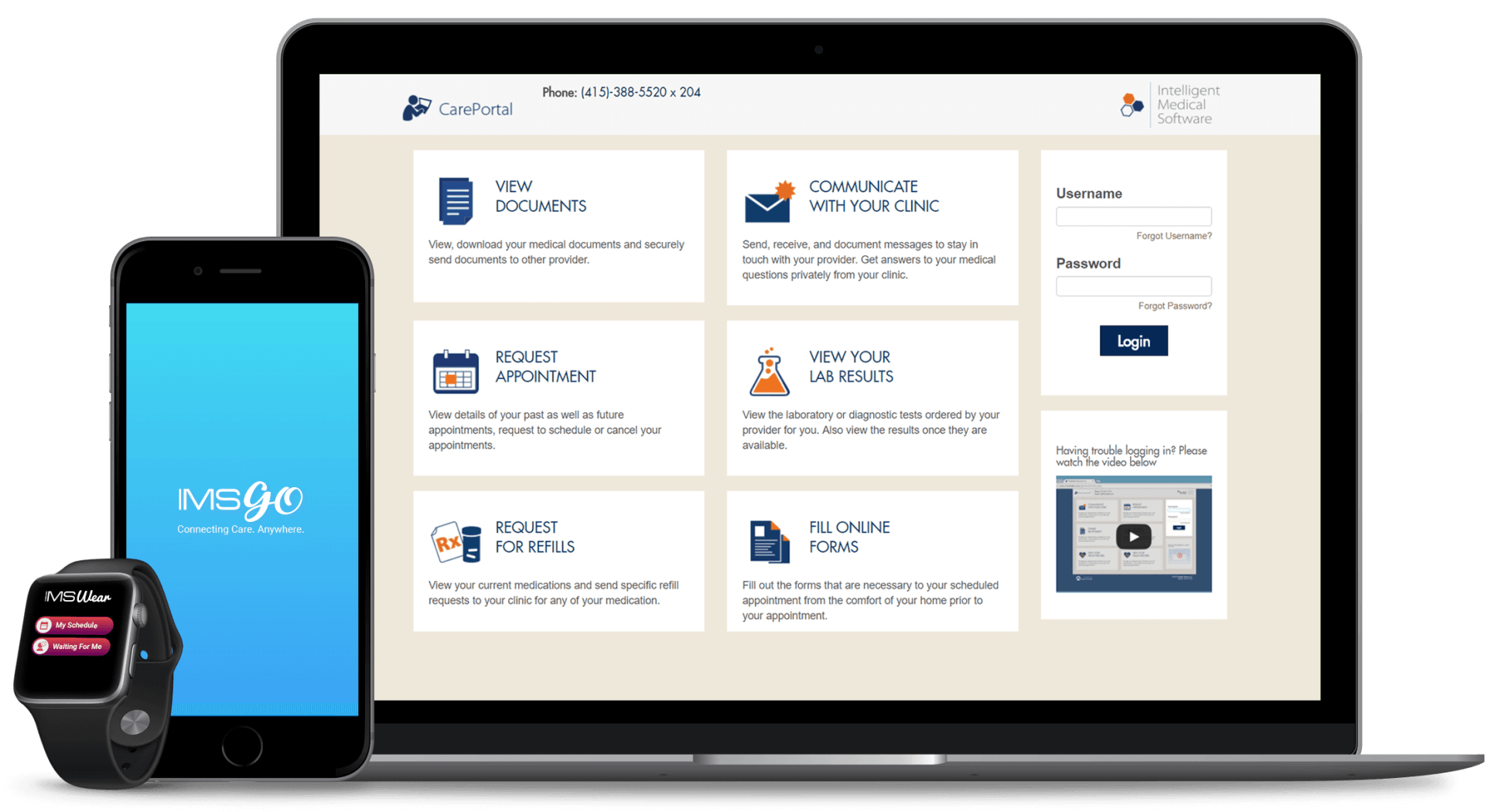
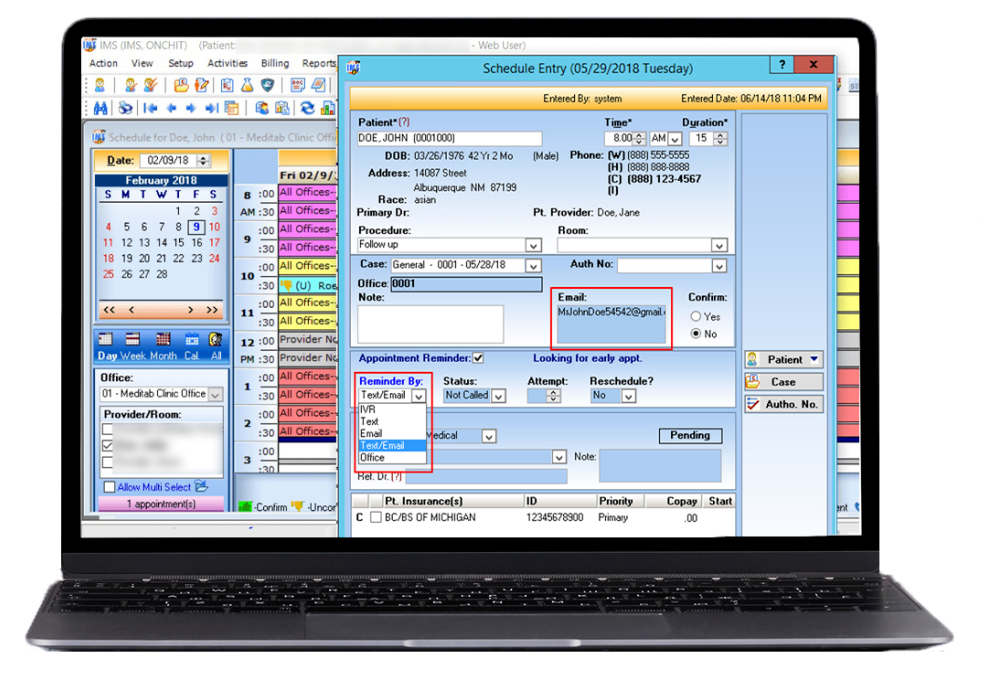
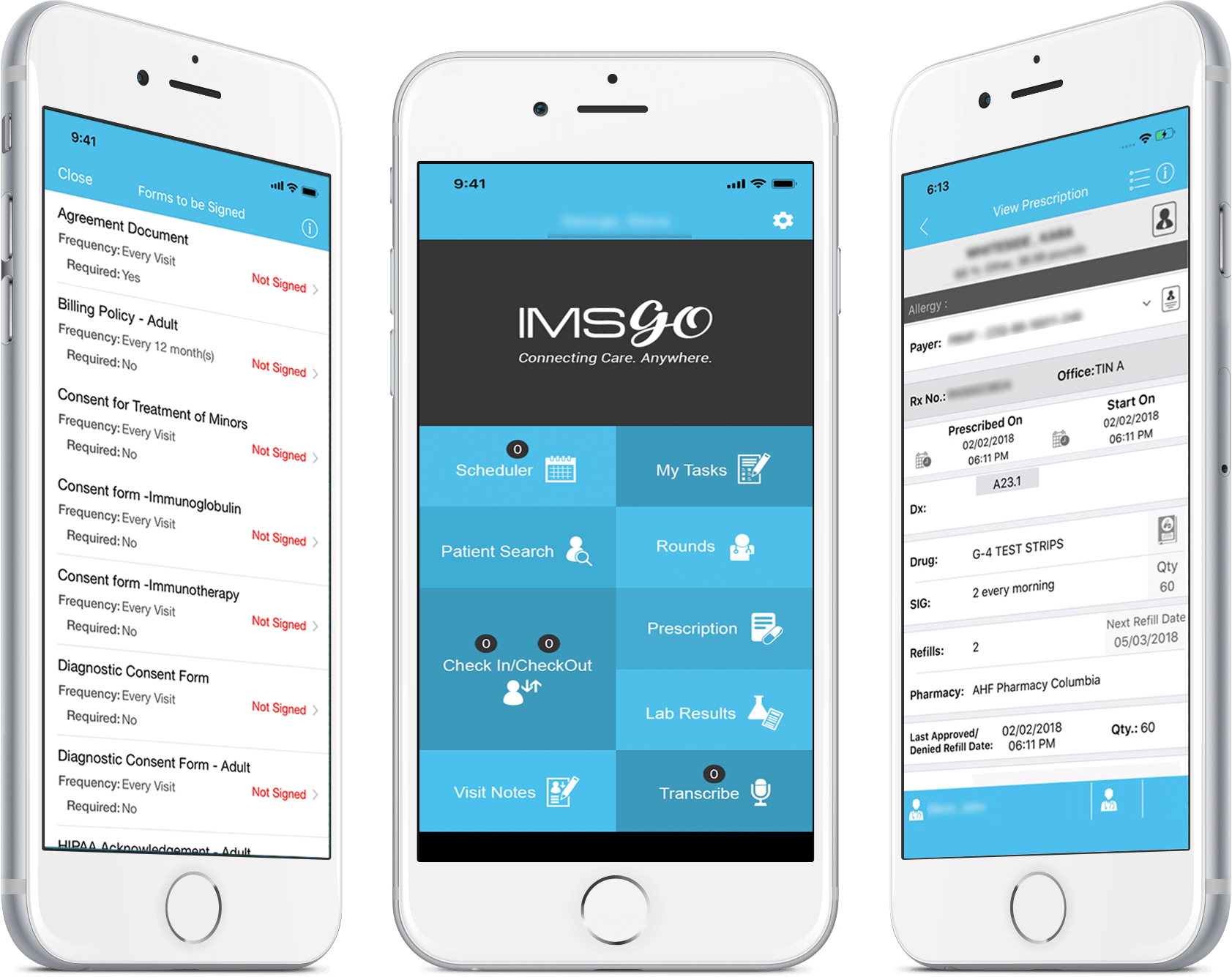
Promoting Interoperability (PI) Measures.
CMS has eliminated the base and performance scoring previously use and went to a New performance-based scoring with four objectives and a maximum of 100 category points.
The four Objectives are:
1. e-Prescribing (with 1 bonus measures) (10 points)
- Query of Prescription Drug Monitoring Program (PDMP) (5 bonus points)
2. Health Information Exchange which has two parts. (40 points total)
- Support Electronic Referral Loops by sending Health Information (20 points)
- Support Electronic Referral Loops by receiving ad incorporating Health Information (20 points)
3. Provider to Patient Exchange (40 points)
- Provide Patients Electronic Access to their Health Information (40 points)
4. Public Health and Clinical Data Exchange (10 points)
- Immunization Registry Reporting
- Electronic Case Reporting
- Public Health Registry Reporting
- Clinical Data Registry Reporting
- Syndromic Surveillance Reporting
Review the Promoting Interoperability measures here.
Improvement Activities (IA) Measures.
For the 2020 reporting, to satisfy this category, ECs can either: attest to completing up to 4 medium-weighted activities or attest to 2 high-weighted activities or attest to 1 high-weighted and 2 medium-weighted activities for a minimum of 90 days. High weighted-activities receive 20 points and medium-weighted activities receive 10 points.
Clinicians with special statuses will receive double points for each high-weighted or medium-weighted activity submitted. They include:
- Small practice
- HPSA providers
- Non-patient Facing
- Rural
Practices that are certified patient-centered medical home (PCMH) will earn the maximum Improvement Activity performance category.
For group reporting, 50% of the clinicians in the group need to attest in performing the same activity during the 90-day period.
CMS also added a new high-weighted activity, COVID-19 Clinical Trials.
Review the available Improvement Activities here.
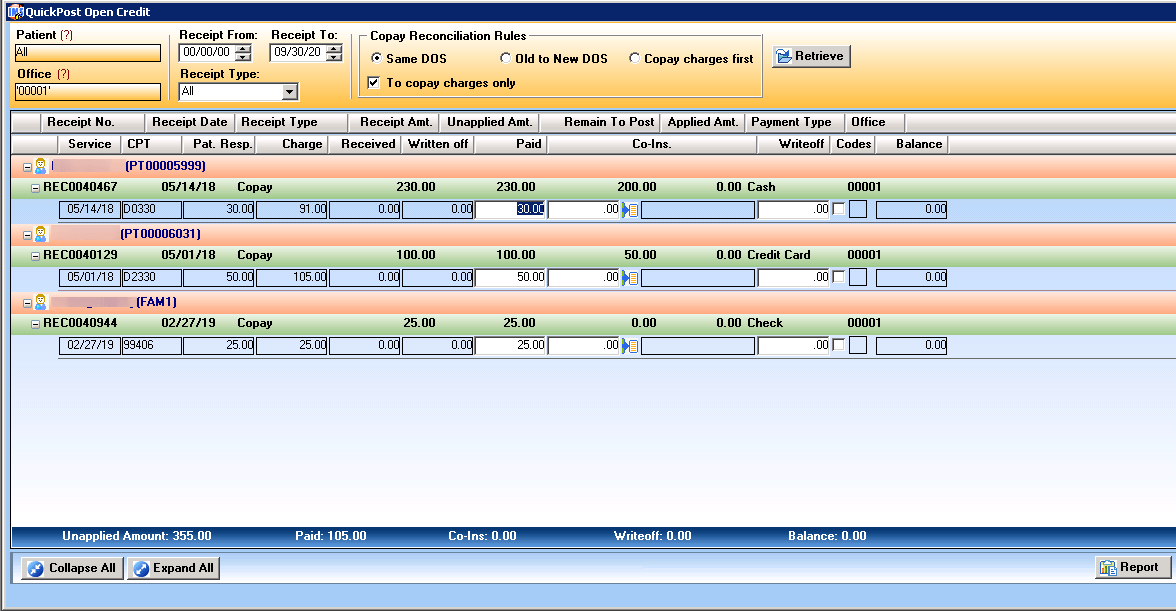
Cost Performance Category.
The Quality MIPS performance category will count for 15% of the total CPS for the 2020 performance period. The 2022 payment adjustment period will be based on your data submitted during the 2020 reporting period.
Cost Measure Case Minimums
- Case minimum of 20 for Total per Capita Cost measure and 35 for MSPB
- Case minimum of 20 for acute inpatient medical condition episodes
- Case minimum of 10 for procedural episodes
For clients, contact us at 1-844-4-Meditab
or qpphelp@meditab.com