MIPS 2024
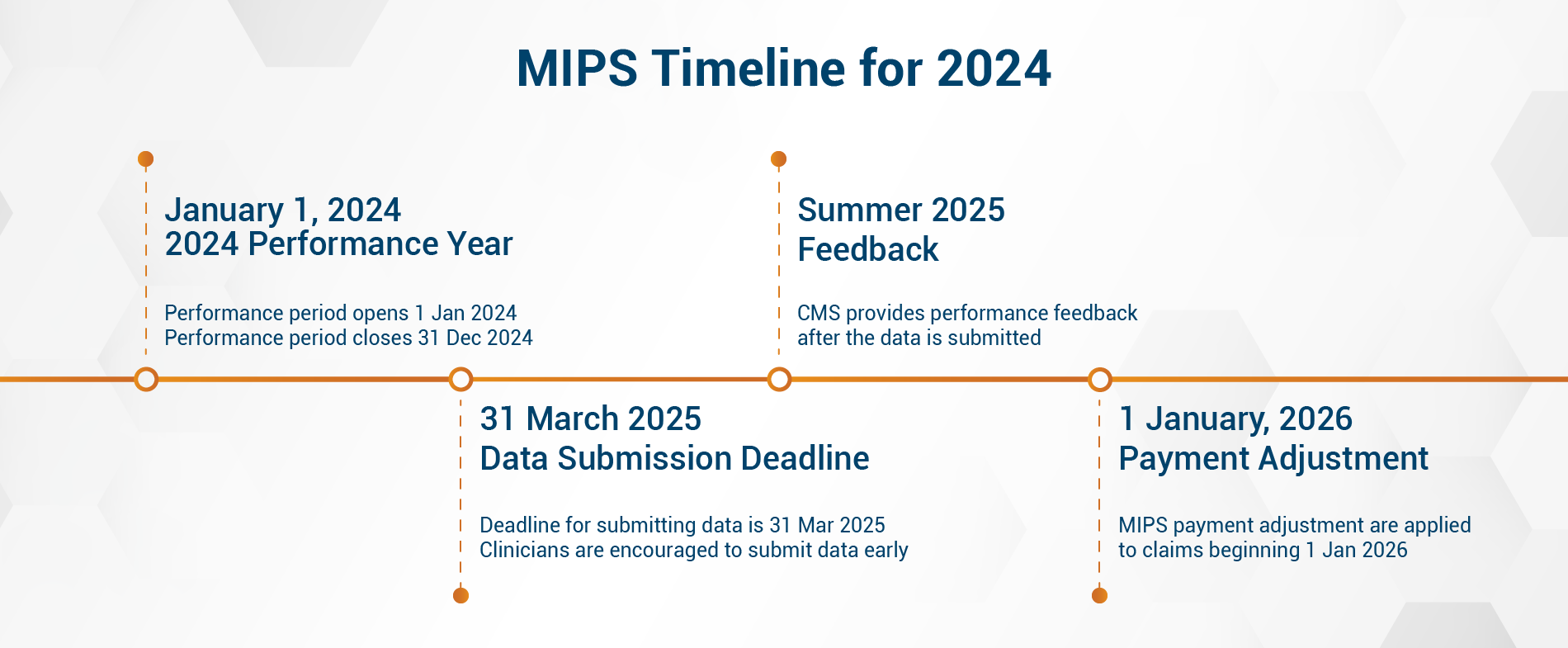
MIPS-eligible clinicians (ECs) must participate and submit their data on or before
March 31, 2025, to avoid a
9% payment penalty. Eligible clinicians, groups, and virtual groups that encountered extreme and uncontrollable circumstances may apply for an exception.
The Extreme and Uncontrollable Circumstances (EUC) exception reweights your MIPS performance categories to as low as 0%. The MIPS EUC exception application for the 2024 performance year will be available until 8 p.m. ET on December 31, 2024.
Our team of attestation experts can help you apply for the EUC exception without the hassle. To learn more about the MIPS 2024 exceptions,
click here.
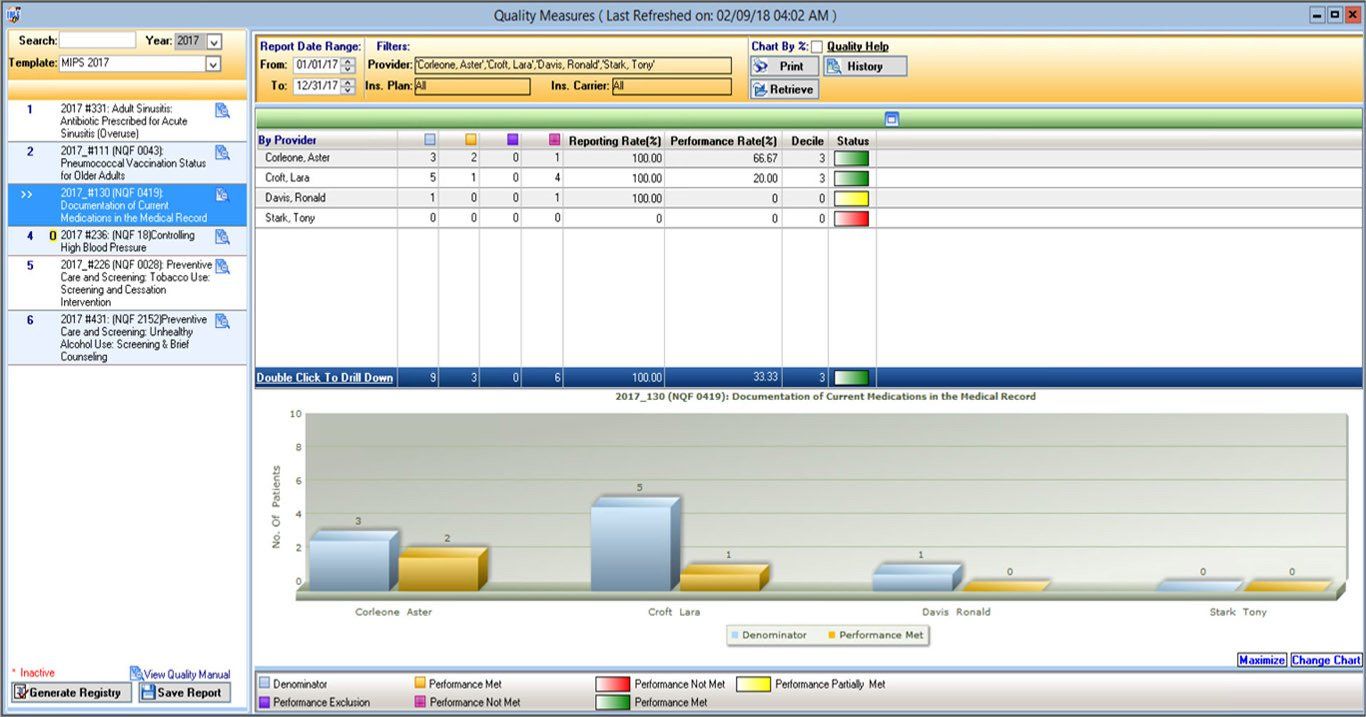
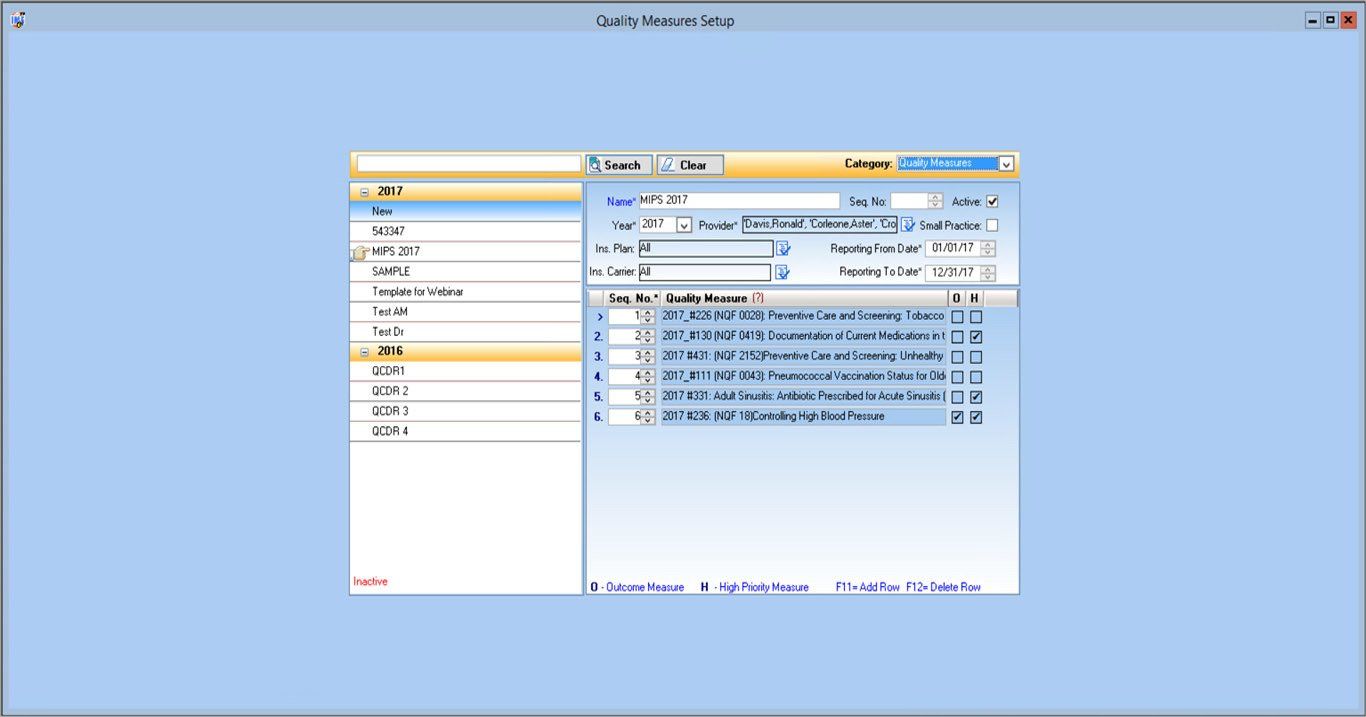
Quality Measures
The Quality performance category accounts for 30% of your final MIPS score over a 12-month performance period (January 1–December 31, 2024).
Eligible clinicians must select 6 individual measures, 1 of which must be an outcome or a high-priority measure. You may also choose to submit data for a specialty measure set that best fits your practice.
- There must be at least 20 cases per measure.
- If fewer than 6 measures apply, then you have to report on each applicable measure.
- Eligible clinicians from small practices (15 or fewer ECs) who submit data on at least 1 quality measure may qualify for the Small Practice bonus and earn 6 points.
- You can also receive up to 10 additional percentage points based on your improvement in the Quality performance category from the previous year.
Instead of the usual 70% data completeness threshold, the Centers for Medicare and Medicaid Services (CMS) now requires you to report performance data for
at least 75%
of the denominator-eligible cases for each quality measure. Measures can generally earn between 1 and 10 points based on the following:
- Your performance if the measures have a benchmark
- If you meet the 75% data completeness threshold
- If you meet the minimum requirement of 20 cases per measure
New Quality measures in their first year have a scoring floor of 7 points, while new Quality measures in their second year have a scoring floor of 5.
Measures that fail to meet the data completeness criteria receive zero points (small practices will continue to receive 3 points).
You can review the available Quality measures
here.
Cost Measures
The Cost performance category accounts for 30% of your final MIPS score over a 12-month performance period (January 1–December 31, 2024).
Qualified participants can continue to earn a 1% improvement score if they have improved their Cost performance category score from the previous year.
Beginning the 2024 performance period, the acute inpatient medical condition measure
Simple Pneumonia with Hospitalization
has been removed from the Cost performance category. On the other hand, the following new episode-based cost measures have been introduced, each with a 20-episode case minimum:
- An acute inpatient medical condition measure (psychoses and related conditions)
- 3 chronic condition measures (depression, heart failure, and low back pain)
- A measure focusing on care provided in the emergency department setting (emergency medicine)
Cost Measure Case Minimums
- Case minimum of 20 for Total per Capita Cost measure and 35 for MSPB
- Case minimum of 20 for acute inpatient medical condition episodes
- Case minimum of 10 for procedural episodes
CMS uses Medicare claims to calculate your Cost measure performance, so you don’t have to submit any data for this category.
To learn more about the Cost measures,
click here.
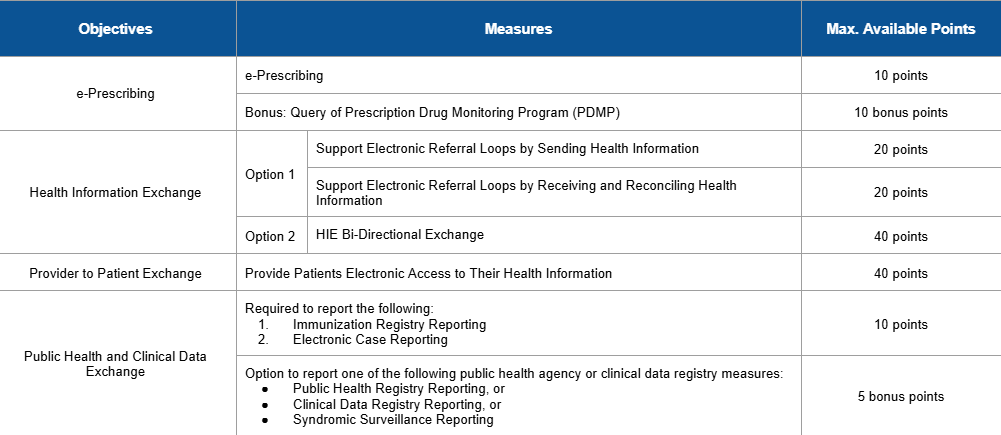
Promoting Interoperability
The Promoting Interoperability (PI) category accounts for 25% of your final MIPS score. Its performance period spans
180 consecutive days in the same performance year, an increase from last year’s 90-day period.
For the 2024 performance year, CMS requires you to use an electronic health record (EHR) that meets the 2015 Edition certification criteria, 2015 Edition Cures Update certification criteria, or a combination of both. You must submit collected data for specific measures from each of the 4 objectives.